The Insurance Claims to Process Report
It's the end of a busy day. You've been checking patients in and out, taking payments, filing insurance claims, answering phones and scheduling appointments. At some point during the day, you even had time to take a lunch break while one of the assistants covered the phones. Now it's time to run the end-of-day reports.
One important report you should be running each day is the Insurance Claims to Process Report. This report will identify all insurance claims that have been created in the Ledger but not printed, as well as those sent to the Batch Processor or sent electronically through eClaims. We all know that sometimes claims slip through the cracks and don't get submitted, and this report is the easiest way to catch them.
When you run this report you can specify a range of patients, providers and insurance carriers to be included. You can also filter using the claim date, type of claim (primary/secondary), patient name, insurance company name, claim amount and expiration date on the report to keep it focused on just the information you are looking for. The report includes total amounts for primary and secondary claims and a combined total to let you know just how important it is that you don't miss submitting these insurance claims.
To generate the Insurance Claims to Process Report:
-
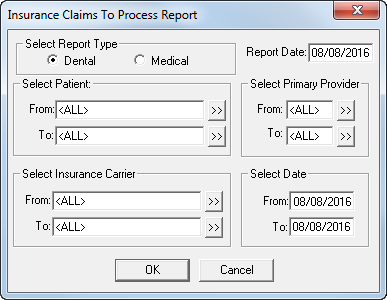
From the Reports menu in the Office Manager, click Ledger > Insurance Claims to Process. The Insurance Claims to Process Report dialog box appears.
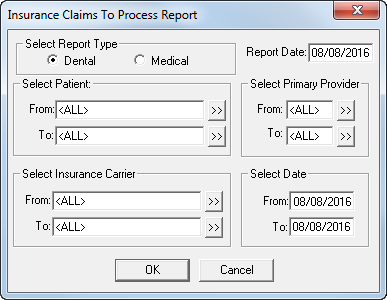
- Select Dental to include dental insurance carriers or Medical to include medical insurance carriers.
- Type the Report Date you want to print on the report. The default is the current date.
-
Do the following:
- Select Patient - Select the range of patients you want to include, using the From and To search fields, or leave <ALL> selected in both fields to include all patients.
- Select Primary Provider - Select the range of providers you want to include, using the From and To search fields, or leave <ALL> selected in both fields to include all providers.
- Select Insurance Carrier - Select the range of carriers you want to include, using the From and To search fields, or leave <ALL> selected in both fields to include all insurance carriers.
- Select Date - Enter the creation date range of insurance claims that you want to include on the report in the From and To fields.
- Click OK to generate the report and send it to the Batch Processor.
Once generated, the report provides the following key elements:
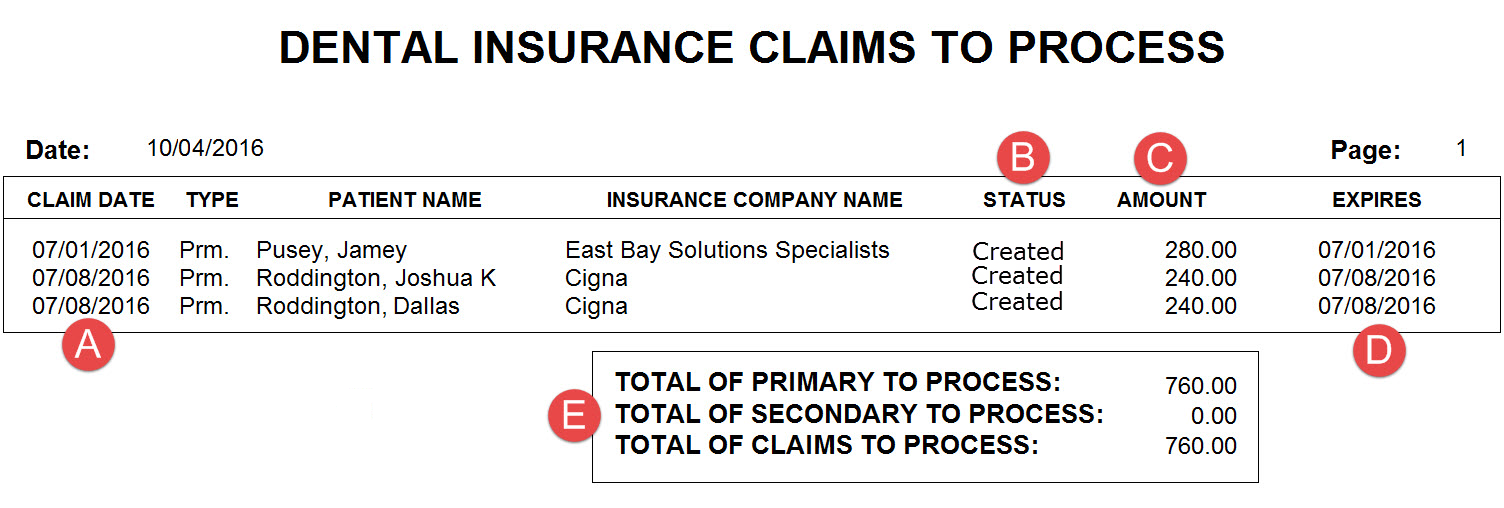
- Claim Date - The date on which the claim was posted to the Ledger.
- Status - The claim status. Because this report includes only claims that have been posted but not processed, each claim displays "Created."
- Amount - The claim amount.
-
Expires - The deadline by which the insurance carrier must receive the claim.
Note: The Expires column pulls the claim expiration date from the Claim Deadline field in the Insurance Coverage dialog box for the insurance plan. If you have not customized this deadline, the expiration date will be the same as the claim creation date. This date is coming from Dentrix and is not necessarily an indication that the insurance company will not pay on the claim. - Totals - The total value of primary and secondary claims.
By generating this report on a regular basis, you can catch unprocessed claims in a timely manner so you can make sure to submit them and get paid.
For additional information on this and other Ledger reports, see the Dentrix Help.
Author: Sean Eyring
Published: 11/30/2016

 Contact Us
Contact Us Phone:
Phone:  Email
Email Request Demo
Request Demo